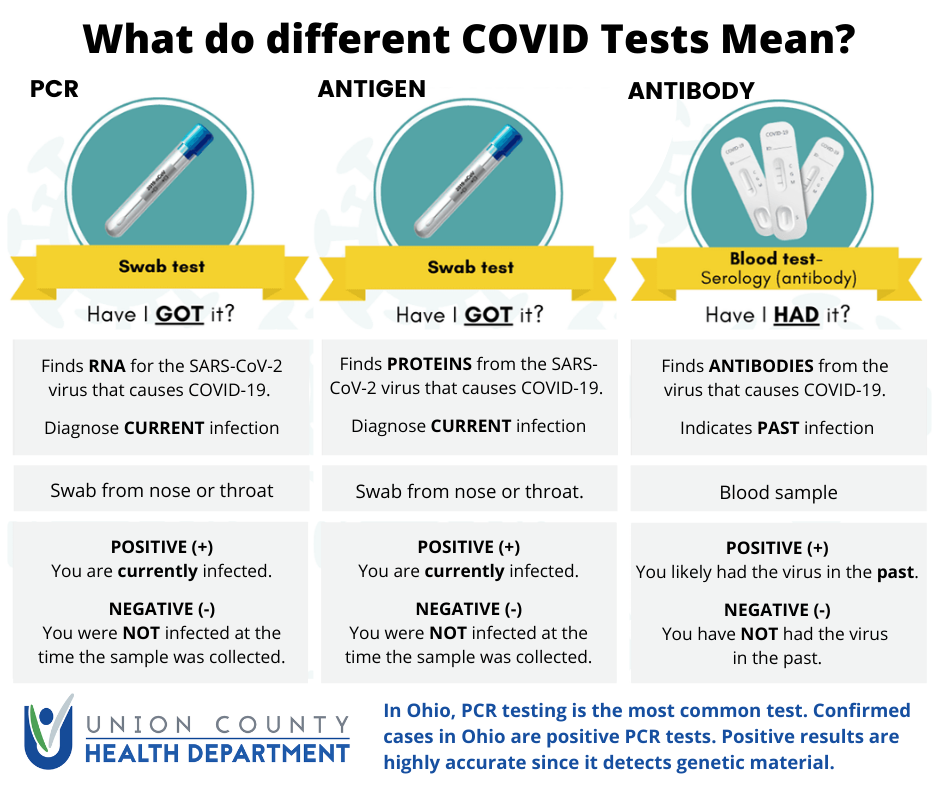
Molecular Test: The most common test type in Ohio is a molecular test that looks for the genetic material of the specific SARS CoV-2 virus that causes COVID-19. This test is called a PCR (polymerase chain reaction) test. This is the test used when we report lab confirmed cases. A sample for testing is collected by a swab in the nose or throat. Results typically take several days. There are some rapid molecular tests termed “Point of Care” that provide results rapidly. However, these rapid “Point of Care” tests are still limited in availability.
Antigen Test: Antigen tests are a newer test that looks for certain proteins from the virus. A sample for testing is collected by a swab in the nose or throat. Results are rapid, available within minutes to hours. This type of test is still not commonly used in Ohio. An individual with a positive antigen test would also need to meet one of two other criteria to be classified as a probable case – clinical evidence of illness (symptoms consistent with COVID-19) or evidence of exposure to a known case.
Antibody Test: Antibody tests, also called serological tests, look for antibodies that indicate a past infection. A blood draw is used for testing. This is the type of test offered by the American Red Cross on blood donations. This test only detects if antibodies have developed, likely from a past infection. This test is not used to diagnose COVID-19. This test also does not mean you have immunity if you have antibodies. Researchers still don’t know if immunity develops after an infection, and if it does, for how long it may protect.